Introduction: The Gut Barrier and Food Allergies
The intestinal barrier, a single layer of epithelial cells connected by tight junctions, plays a crucial role in maintaining homeostasis. It selectively allows essential nutrients to pass into the bloodstream while preventing the entry of harmful substances, including undigested food particles and pathogens. When this barrier is compromised, leading to increased intestinal permeability (often referred to as 'leaky gut'), it can trigger a cascade of immune responses that may contribute to the development of food allergies.
What is Intestinal Permeability?

Intestinal permeability refers to the controlled movement of substances across the intestinal wall. This is primarily regulated by tight junction proteins like occludin, claudins, and zonulin. Dysregulation of these proteins can lead to increased permeability, allowing larger molecules to cross the barrier. Zonulin, in particular, has been identified as a key modulator of tight junctions. Elevated levels of zonulin can directly impact gut permeability.
Increased Intestinal Permeability:
Gut Health --> Compromised Tight Junctions --> Larger Molecules Leak --> Immune Response
Decreased Intestinal Permeability:
Gut Health --> Intact Tight Junctions --> Selective Absorption --> Maintained HomeostasisThe Role of Zonulin in Leaky Gut
Zonulin is a protein that modulates the permeability of tight junctions between cells of the digestive tract. It is released in response to stimuli such as bacteria or gluten. Elevated zonulin levels disrupt tight junctions, leading to increased intestinal permeability. This allows undigested food particles and bacterial components to enter the bloodstream, potentially triggering an immune response and contributing to food allergies.
Immune Response to Increased Permeability
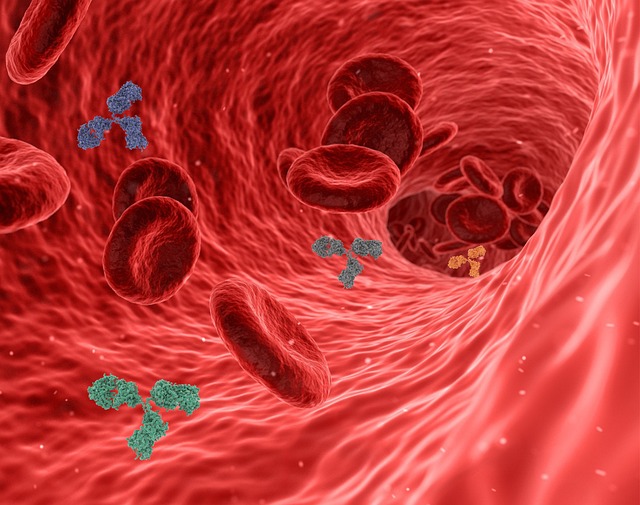
When undigested food particles cross the intestinal barrier, they are recognized as foreign antigens by the immune system. This triggers an immune response, leading to the production of antibodies (IgE, IgG, etc.) and the activation of immune cells. Chronic exposure to these antigens can lead to sensitization and the development of food allergies. The type of immune response (e.g., Th1 vs. Th2) can also influence the manifestation of allergic symptoms.
Factors Influencing Intestinal Permeability
- Diet (e.g., gluten, processed foods)
- Stress
- Infections (bacterial, viral, parasitic)
- Medications (e.g., NSAIDs)
- Genetics
- Dysbiosis (imbalance in gut microbiota)
Potential Therapeutic Strategies

Targeting the underlying causes of increased intestinal permeability is crucial for managing food allergies. Potential therapeutic strategies include:
- Dietary modifications (e.g., elimination diets, anti-inflammatory diets)
- Probiotic supplementation to restore gut microbiota balance
- Prebiotic supplementation to nourish beneficial gut bacteria
- L-Glutamine supplementation to support intestinal cell health
- Stress management techniques
- Targeted therapies to reduce zonulin production or enhance tight junction integrity