Introduction: The Gut-Brain Axis and IBS
Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder characterized by abdominal pain, bloating, and altered bowel habits. While the exact cause remains elusive, growing evidence points to the critical role of the gut-brain axis (GBA). The GBA is a bidirectional communication network connecting the central nervous system (CNS) and the enteric nervous system (ENS), the 'brain' of the gut. This intricate interplay involves neural, hormonal, and immunological signaling pathways.
The Gut Microbiota: A Key Player in GBA Communication
The gut microbiota, the diverse community of microorganisms residing in the gastrointestinal tract, significantly influences GBA communication. Dysbiosis, an imbalance in the gut microbiota composition, has been frequently observed in IBS patients. Specific microbial species can produce neurotransmitters like serotonin and gamma-aminobutyric acid (GABA), directly impacting brain function. Furthermore, microbial metabolites, such as short-chain fatty acids (SCFAs), can modulate inflammation and gut permeability, indirectly affecting the CNS.
# Example: Estimating microbial diversity (alpha diversity) using Shannon index
import numpy as np
from scipy.stats import entropy
def shannon_diversity(counts):
"""Calculates the Shannon diversity index."""
counts = np.array(counts)
relative_abundance = counts / np.sum(counts)
return entropy(relative_abundance, base=np.e)
# Example microbial counts
microbial_counts = [100, 50, 25, 10, 5]
diversity = shannon_diversity(microbial_counts)
print(f"Shannon Diversity Index: {diversity}")Visceral Hypersensitivity and Altered Sensory Processing
A hallmark of IBS is visceral hypersensitivity, an increased sensitivity to pain or discomfort in the internal organs. Altered GBA communication can lead to increased neuronal excitability in the gut and spinal cord, amplifying pain signals transmitted to the brain. Furthermore, central nervous system processing of visceral stimuli may be dysregulated in IBS, contributing to heightened pain perception.
Immune Activation and Inflammation
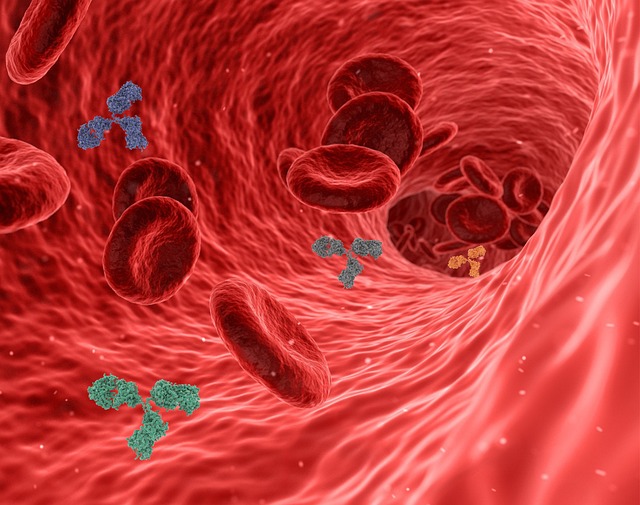
Low-grade inflammation in the gut is increasingly recognized as a factor in IBS. The gut microbiota can trigger immune responses, leading to the release of inflammatory cytokines. These cytokines can affect the enteric nervous system and also cross the blood-brain barrier, influencing brain function and contributing to symptoms like anxiety and depression, which are commonly comorbid with IBS.
Stress and the Gut-Brain Axis: A Vicious Cycle
Stress significantly impacts the GBA, exacerbating IBS symptoms. Psychological stress can alter gut motility, increase gut permeability, and influence the composition of the gut microbiota. These changes, in turn, can further dysregulate GBA communication, creating a vicious cycle of stress and gut dysfunction. The hypothalamic-pituitary-adrenal (HPA) axis, a key stress response system, is intimately connected to the GBA. Activation of the HPA axis releases cortisol, which can directly affect gut function.
Therapeutic Strategies Targeting the Gut-Brain Axis

Given the central role of the GBA in IBS, therapeutic strategies aimed at modulating this axis are gaining increasing attention. These include: * **Dietary interventions:** Low-FODMAP diets and other dietary modifications can reduce gut fermentation and alleviate symptoms. * **Probiotics and prebiotics:** These can modulate the gut microbiota composition and improve GBA communication. * **Psychological therapies:** Cognitive behavioral therapy (CBT) and other psychological interventions can help manage stress and anxiety, indirectly impacting gut function. * **Pharmacological agents:** Medications targeting specific neurotransmitter pathways or inflammation may be beneficial.
Further Reading and Scientific Research
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): https://www.niddk.nih.gov/
- The Rome Foundation: https://theromefoundation.org/
- PubMed: https://pubmed.ncbi.nlm.nih.gov/
